8 menstrual facts you didn’t know
A couple of months ago, I decided to start writing a series of posts on menstruation. My previous articles Menstruation series: an introduction and All you need to know about menstrual products were very well received.
Today, I’d like to tell you some facts I’ve learned about periods since I started working as a translator specialized in women’s health.
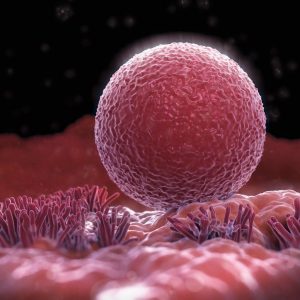
The egg does not leave your body with your menstruation
How many times have you tried to find your unfertilized egg in your menstrual blood? If you’ve searched for it and you even confused it with a menstrual clot, you’re not the only one. This myth is extremely common. Luckily, I’ve recently learned thanks to Xuxa Sanz, (you can follow her on Instagram) that this information is incorrect. In Xuxa’s words, “the unfertilized egg does not travel to your uterus. Instead, it dies in the fallopian tube and it is destroyed and reabsorbed by macrophages. Your egg does not travel up to your uterus unless it is fertilized. If so, it will be placed in your uterus and stay there to continue with a pregnancy.”
Menstrual pain is NOT normal

If you actually think about it, why would it be normal to feel pain? There’s always an underlying cause whenever you’re in pain. For example, if you have a headache, you might be too stressed or you may have a bad posture; if you have a toothache, you might have a tooth decay. So, why are we told that period pain is normal?
Our menstrual cycle is a vital sign and it should be treated as such. Having this in mind, menstrual pain must have an underlying cause, just like all other kinds of pain. Have you ever noticed that some of your cycles are more painful than others? According to Dr. Lara Briden, “as your uterine lining starts to break down at the end of your cycle, it releases prostaglandins. They stimulate your uterine muscle to contract to help to shed the lining. Prostaglandins are a normal part of the process, but too many prostaglandins can cause pain.” This means that we should attempt to reduce prostaglandins.
Note: if your menstrual pain is so strong that you cannot have a normal life or if it does not get better after taking a painkiller, you might have a more serious disease like adenomyosis or endometriosis and you should see a doctor.
PMS can be treated and solved
I’m talking about the well-known premenstrual syndrome that affects most women during their fertile life. Have you experienced anxiety, mood swings, breast tenderness or food cravings on the days before you start menstruating? Dr. Briden has a whole chapter of her book Period Repair Manual —I had the honor of translating this book into Spanish— to suggest a natural treatment for premenstrual syndrome. In my case, ever since I started taking magnesium and vitamin B6, my PMS symptoms have improved a lot.
Ovulation is the most important part of your cycle
I’ve always thought that the most important part of my cycle was bleeding. Have you thought the same? You’re not alone. Now I know that the star of my cycle is ovulation. According to Jerilynn Prior, “ovulatory cycles are both indicators and creators of health.”
Ovulation indicates that your body is working properly. That is, you’re well-fed, you can handle stress, your thyroid hormone works well and your insulin levels are not too high. Everything is fine.
Ovulation creates health because this is the way your body has to produce progesterone. You should think about your monthly dose of progesterone as a deposit in the bank of your health. Ovulation generates a reserve of progesterone for your bones and metabolism that will ease your journey through menopause. (That’s why it’s so important to ovulate during your reproductive years and you shouldn’t be blocking ovulation with hormonal contraceptives.)
Hormonal contraceptives have more side effects than benefits

Hormonal contraceptives (pill, mini-pill, vaginal ring, patch, injection, hormonal IUD) have one main goal: to avoid ovulation so that you cannot get pregnant. Apart from the fact that they “switch off” your hormones, you are at risk of:
- Blood clots
- Depression
- Libido loss
- Hair loss
- Weight gain
- High blood pressure
- Nutrient deficiency
- Reduced thyroid function
Have you ever been told that when you are on hormonal birth control your skin and hair will look so much better? Or have you been told that you will no longer suffer from period pain or heavy bleeding? Besides all the side effects mentioned above, your health might be affected when you stop hormonal birth control. Problems such as post-pill acne, post-pill PMS and post-pill amenorrhea are fairly common and it can take months to recover your normal cycle.
Source: Period Repair Manual, chapter 2.
PCOS and HA are far more common than I thought
Polycystic ovary syndrome (PCOS) and hypothalamic amenorrhea (HA) are two concepts that I didn’t even know before specializing in women’s health. After working with Dr. Briden and with the authors of paleosop.com, I learned that many women are thrilled when their menstruation comes.
According to Dr. Briden, “PCOS is a common diagnosis that affects up to 10 percent of women. It’s best defined as a group of symptoms related to anovulation (lack of ovulation) and a high level of androgens or male hormones. The main symptom of PCOS is irregular periods, specifically late periods or too many days of bleeding. Irregular periods are typical of anovulatory cycles.
Hypothalamic amenorrhea is defined as the lack of a menstrual period for more than six months when no medical diagnosis can be found.”
There are great alternatives for a sustainable menstruation

For a long time I felt guilty thinking about the environmental impact of my period. Did you know that an average woman generates waste equivalent to 10000 tampons and/or pads during their fertile life? Just thinking about this number gives me the chills.
Fortunately, there are many options to have a sustainable menstruation. Women from ilovecyclo work tirelessly to promote the use of reusable menstrual products. You can read more about this here. I started using the menstrual cup several months ago and it’s the best decision I’ve made in years.
We don’t ovulate every month with a different ovary
I also learned this from Xuxa Sanz. “Ovulation is not a lateral action, there is no specific mechanism indicating the left or right ovary to ovulate every month. It is said that we ovulate every month with a different ovary because it is believed that during our fertile life we ovulate 50% with every ovary. However, it is not rare for a woman to ovulate 3 month in a row with the same ovary. Actually, women with only one ovary can ovulate and have their periods every month.”
What do you think? Do you feel that you’ve learnt anything new? Is there anything you’d like to add? Share your thoughts in the comments!
Hi! I’m Ariadna from ariadnatranslations.com

I’m here to share some thoughts and ideas about my job as a translator. I love writing about language, women/feminism, health and wellbeing, among other interesting topics. If you liked what you read above, I invite you to comment and share in your social media. Let’s all learn from each other! Remember: sharing is caring!
1 comment so far